In 2012, a few days after Katie Rich gave birth to her third child, she started experiencing sharp pains under her ribs. When she brought it up at her postpartum checkup, her doctor thought it might be Rich’s gallbladder. Instead a sonogram revealed a spot the size of a dollar bill on her liver. It might be a bruise, her doctor told her. “You are 33 years old. Do not worry about this,” she remembers him saying.
Rich did not have time to worry. Her oldest child was three, and her newborn was only eight weeks. “We were so overwhelmed with the three little kids,” she says. But she did follow up. A biopsy revealed stage IV colon cancer. Rich got the call on a Friday and spent the weekend crying. “I was in total disbelief,” she says.
The diagnosis made no sense to her. Nobody in her family had ever had colon cancer. Rich, an athlete, ran and played volleyball. She exercised through all of her pregnancies. She made sure to eat a healthy diet. And she was young. Colon cancer was not even on her radar.
Stories like Rich’s are increasingly common. Even as colorectal cancer rates for older adults have declined, rates in younger people have started climbing. In 2010 adults younger than 50 accounted for 5 percent of colon cancers and 9 percent of rectal cancers. By 2020 those proportions had grown to 11 and 15 percent, respectively.
The underlying reasons for this rise remain a mystery, one that is proving increasingly frustrating for those in the field. Experts now recommend that the general public start screening at age 45 instead of 50, a stopgap measure that they hope will identify many of these cases. But it is hardly a perfect fix. The new guidelines will not catch the increasing number of cases in people younger than 45—people like Rich. And some worry that the influx of newly eligible adults could strain the system and divert resources toward younger, healthier people and away from older adults in underserved populations, who are already less likely to be screened. If researchers could figure out who is at greatest risk, they could target those individuals for screening. The reality, however, is that the constellation of factors that are putting more younger people at risk has proved difficult to pin down.
Rising Rates
Cancer screening is designed to identify disease before someone develops symptoms. The rationale is simple: cancer is easier to treat when it is diagnosed early. And colorectal cancer screenings in particular can prevent cancer from ever taking hold. During a colonoscopy, doctors examine the colon with a flexible scope that allows them to take biopsies and remove precancerous polyps. These screenings have led to an overall decrease in colorectal cancer incidence and mortality—so much so that declines in the disease have often been touted as progress in the war on cancer.
But that progress masks a disturbing trend. In 2008 Rebecca Siegel was mired in data, deep in the latest update of a report by the American Cancer Society called “Cancer Facts and Figures.” Siegel, a cancer epidemiologist with ACS, had run the numbers before. At the time the recommendation was that screening should begin at 50 for adults with no obvious risk factors. What would happen, she wondered, if someone broke down the numbers in a slightly different way and instead looked at incidence among people younger than 50?
To her surprise, that analysis showed that colorectal cancer rates were going up. Between 1992 and 2005 the overall incidence for people 20 to 49 years old increased 1.5 percent a year in men and 1.6 percent a year in women. (The rise was largely driven by rectal cancer, which rose 3.5 percent a year in men and 2.9 percent a year in women.) The numbers were even more stark when she broke them down by race: Per year, incidence had increased among white men by 2.0 percent and in white women by 2.2 percent. There was no statistically significant change in Hispanic women, but she found an increase in Hispanic men of 2.7 percent a year. The absolute risk for these younger people was small compared with the risk for older people, but Siegel found the trend troubling.
Declines in disease in the over-50 age groups had made it appear that colorectal cancer incidence was going down overall. But, Siegel says, “What’s going on in the younger age groups is really masked.”
Siegel published her results in 2009. “It got a little bit of attention,” she says, but reactions were mixed. The consensus at the time was that screening should begin at 50. Rather than seeing Siegel’s results as concerning, some argued that the increase was probably good news and attributed it to more young people being screened.
Siegel did not buy it. She points out that if the increase were the result of more screening, doctors would be catching more early-stage cancers and seeing declining mortality rates in this younger group. Instead, as she collected more data over the next eight years, she found more late-stage diagnoses and mortality rates that were climbing by about 1 percent a year.
In 2017, as evidence for rising rates piled up, the ACS’s Guideline Development Group began to reassess its screening guidelines for colorectal cancer, tweaking models to incorporate increasing incidence among younger adults. When it lowered the age to 45, the benefits outweighed the harms. ACS updated its recommendations accordingly the following year.
The move “caused quite a stir,” says Aasma Shaukat, a gastroenterologist at New York University’s Grossman School of Medicine. At the time critics argued that colorectal cancer affects too few younger adults to warrant the change. Even today the risk of someone in their late 70s being diagnosed with colon cancer is about one in 500, whereas the risk for someone in their early 30s is about one in 17,500. And, the same critics said, there were not enough data to support such a shift in recommendations.
A Puzzle Unsolved
Today it is clear that the increase in early-onset colorectal cancer is real. In the 20-to-49 age group, rates climbed from about one in 12,000 in 1992 to one in 9,300 in 2015. “It’s not just a blip,” says Folasade P. May, a gastroenterologist at the University of California, Los Angeles. Some groups have been hit harder than others. The upward trend has been steepest among people who are white, Native American and Alaska Native.
Black people have had higher rates of colorectal cancer across all age groups for decades. “We still see young-onset colorectal cancer in Black individuals,” May says, “but they were already having those high rates.” Mortality rates are highest in these groups, too. But in adults younger than 50, she says, it is white men who are driving the increase. Twenty-five years ago Black people between 20 and 49 years old had a 40 percent higher incidence of colorectal cancer than white people in the same age group. As of 2016, the two groups were the same: one in 7,000.
Exactly what factors are prompting this rise is still unknown, but they are apparently increasing with each generation. In the U.S., people born in the 1950s have the lowest incidence of colorectal cancer, and rates rise from there. Someone who is 41 today has a 47 percent higher risk of colorectal cancer than someone who was 41 in 1991—over those 30 years the rate increased from 10.6 to 15.6 people per 100,000. In other words, the risk goes up with every subsequent generation and travels with those individuals as they age, something known as a birth-cohort effect. Other wealthy countries are experiencing similar increases. Siegel and her colleagues looked at rates worldwide and found that during the most recent decade of available data, trends in eight other countries resembled those in the U.S., with incidence increasing among people younger than 50 and stable or decreasing in those 50 and older. Rates among younger adults declined in only three countries: Austria, Italy and Lithuania. Two of those, Austria and Italy, initiate colorectal cancer screening for average-risk adults in their 40s, the very group driving those declining rates.
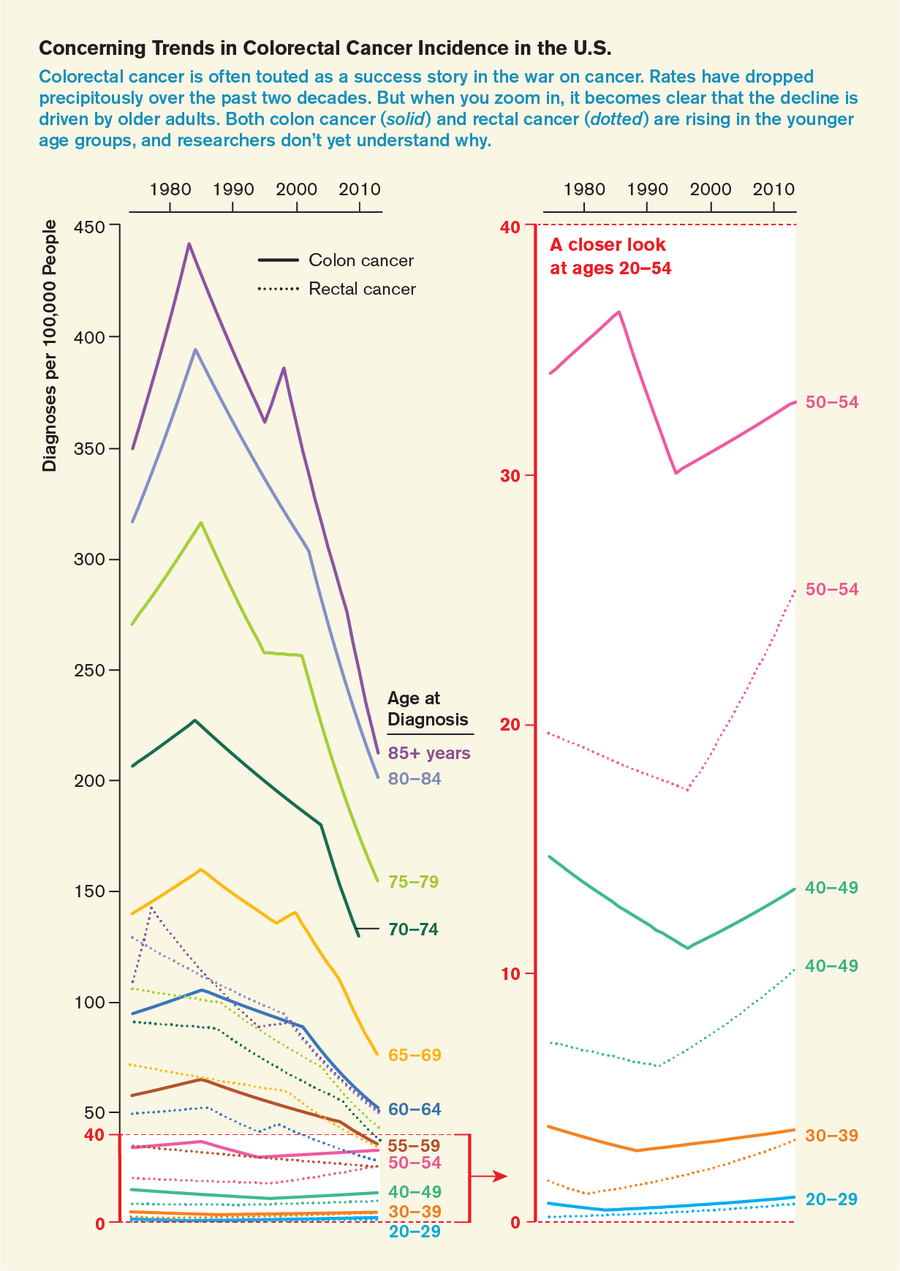
Credit: Jen Christiansen; Source: “Colorectal Cancer Incidence Patterns in the United States, 1974–2013,” by Rebecca L. Siegel et al., in Journal of the National Cancer Institute, Vol. 109; August 2017 (data)
Researchers are scrutinizing the usual suspects—obesity, sedentary lifestyle, smoking, alcohol, diets rich in red meat and processed foods. One study showed that diabetes might play a role. Another found a link to sugary drinks. But for Rich and many others, those explanations do not fit. Actor Chadwick Boseman, who died of colon cancer last year at age 43, “was not obese. He was not sedentary,” says Kimmie Ng, director of the Young-Onset Colorectal Cancer Center at the Dana-Farber Cancer Institute in Boston. “And that is reflective of so many of the young patients we see in our center.”
Some researchers speculate that human papillomavirus (HPV), the cause of most anal cancers, may explain some of the rise in colorectal cancers in younger adults. That would mean that the vaccines that prevent other HPV-caused cancers might be protective. But most research to date has been unable to conclusively make the connection, and more research is needed to confirm or rule out the link.
Because the birth-cohort effect in cancer suggests that exposures early in life, during childhood or young adulthood, may be crucial, some have begun looking closely at changes to the microbiome. “We know that diet and lifestyle significantly shape our microbiome. They also significantly shape our immune system, which we need to fight off the development of cancer. And so we are hypothesizing that it’s a complex interplay among the microbiome, diet, lifestyle and your immune system,” Ng says.
Several case-control studies suggest that antibiotic use may be partly to blame. These medications can have a profound impact on the gut microbiome, potentially tweaking it in ways that foster carcinogenesis. And prescriptions for broad-spectrum antibiotics nearly tripled from 1980 to 1992. One study presented at the 2021 European Society for Medical Oncology World Congress on Gastrointestinal Cancer found that antibiotic use was associated with an increased risk of both early- and late-onset colon cancer.
Another potential explanation that some are exploring is gestational influence. Caitlin Murphy, an epidemiologist at the University of Texas Health Science Center at Houston, and her colleagues have been studying the effect of prenatal exposures on colorectal cancer risk. In a cohort of about 14,500 mothers and their children, maternal obesity increased a child’s future risk of colorectal cancer. High weight gain during pregnancy also contributed to the child’s risk.
That might be one piece of the puzzle, Murphy says, but it is certainly not the only one. “When I first started working in this area, I was kind of convinced that there was this smoking gun,” she says. “The more I get into it, the more I realize that’s just not true.” Figuring out how the pieces fit together and who is most at risk will be essential for screening to be used to best effect.
Screening Debate
There is a growing consensus that the benefits of starting colon cancer screening at age 45 may outweigh potential harms. The American College of Gastroenterology, the National Comprehensive Cancer Network and now the U.S. Preventive Services Task Force have all endorsed the new lowered screening age. The U.S. Multi-Society Task Force on Colorectal Cancer, which is in the process of updating its guidelines, has also adopted the lower age for average-risk adults. (Those with a family history are advised to start screening even earlier.)
Lowering the age to 45 “really does make sense,” Ng says. Because half of early-onset colorectal cancer cases occur in patients in their 40s, she says, “we will catch a lot more cancer in that earlier stage.” At least one study hints that this may be true and that colorectal cancer incidence among people in their 40s might be even higher than anyone thought. A paper published in 2020 in JAMA Network Open reports an odd jump in the number of cases at age 50 compared with age 49. “That’s not because there is something biologically different between 49- and 50-year-olds,” says Swati G. Patel, a gastroenterologist at the University of Colorado Anschutz Medical Center, who was not involved in the study. Rather it is because when people start getting screened, cancers they may have had for years are detected.
The new screening guidelines should help doctors catch some of these cancers. Most adults younger than 50 have never been screened for colorectal cancer and can be slow to seek medical attention. One study found that for patients older than 50, a month passed from the onset of their first symptom to treatment. But for those younger than 50, the median delay was 217 days. Because they were not in the screening group and did not interpret the symptom as a potential problem, they waited to seek care or, if they did consult doctors, their physicians sometimes attributed their symptoms to something else such as hemorrhoids or fistulas.
Some researchers see the move to 45 as premature. If you look at the results of the modeling, Shaukat says, “the risk-benefit ratio is very, very thin.” Screening programs are costly, and colonoscopies are not without risk. Scopes can cause bleeding or even perforate the bowel, something that occurs in about one of every 2,500 procedures. Plus, colonoscopies almost always require sedation, which may have its own complications. Stool tests can yield false positives—rates as high as 13 percent—which induce anxiety and lead to unnecessary procedures.
Increased screening poses hazards not just to individuals but to the entire system. Lowering the screening age by five years means 21 million people are newly eligible for screening. Many clinics already have a hefty screening backlog after halting colonoscopies as COVID cases surged in the spring and fall of 2020. Even where the procedure was available, some opted to postpone out of fear of exposure to the virus.
Now gastroenterologists must find a way to accommodate both the COVID backlog and people in their late 40s. If all these new recruits immediately schedule colonoscopies, they could overwhelm the system and lead to longer wait times for older patients who might have a more acute need. And screening compliance is already below what it should be in the over-50 crowd. According to Murphy’s research from 2018, about 50 percent of white and Black adults in their early 50s are up-to-date with screening, compared with only about 35 percent of Hispanic and 32 percent of Asian adults the same age. And, as Shaukat points out, the healthiest and wealthiest adults in their 40s—executives who run marathons and eat kale—may be the ones who come in for screening first.
There might be a way to strike a balance. At-home stool tests can also detect colorectal cancer, and Siegel believes they should be more widely adopted. One system using them is Kaiser Permanente Northern California, which mails patients annual fecal immunochemical tests—FITs for short—if they are not up-to-date with their screening. These tests detect blood in the stool, something that can be a sign of cancer or precancerous polyps. Only those with positive results need to follow up, typically with a colonoscopy. Since Kaiser launched the program in 2006, the percentage of eligible adults in their system who get screened has increased from 40 percent to more than 80 percent. The national screening rate, in contrast, is just under 69 percent. Even better, cases of colorectal cancer fell by 26 percent among Kaiser’s patients, and deaths related to colorectal cancer dropped by 52 percent.
The Veterans Health Administration has adopted FITs, too. When the pandemic hit, VA hospitals stopped performing screening colonoscopies for veterans with an average risk of colorectal cancer and instead began offering them a home stool test.
Siegel wishes more doctors would offer their patients stool tests as an option. “You don’t have to get a colonoscopy. You can have a test that’s less invasive,” she says. “The reduction in mortality from colorectal cancer is comparable for both.”
A newer test, Cologuard, combines FIT with DNA markers indicative of cancer. But although a single Cologuard test can detect up to 92 percent of cancers, compared with the FIT’s 74 percent, it is much more costly and yields more false positives. Because it is recommended every three years rather than annually, the difference in accuracy over time may be negligible.
Neither test will help adults not yet eligible to be screened. “The rate of rise is actually the steepest in people in their 20s and 30s,” Ng says. Colon cancer incidence is increasing by 2 percent a year in people 20 to 29 years old, compared with 1.3 percent in those 40 to 49 years old. Rectal cancer incidence is rising by 3.2 and 2.3 percent a year in those same groups. That is why we must figure out why rates are increasing. If researchers can determine those most at risk, she says, “we can target them for early screening rather than lowering the age.”
Rich does not know why she got colon cancer so young and tries not to dwell on it. After her weekend crying jag when she was diagnosed, “I never looked back,” she says. She put her energy into the fight ahead. After eight rounds of chemotherapy and the loss of 30 percent of her colon and 70 percent of her liver, Rich has been free of cancer for more than eight years. In 2015 she and her husband had another baby, a girl they named Hope. The chance the cancer will come back is small, but Rich still has an implanted pump her doctors can use to send chemo directly to her liver if it does return. “It’s basically an insurance plan,” she says.
This article is part of “Innovations In: Cancer Early Detection,” an editorially independent special report that was produced with financial support from Johnson & Johnson.